This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.

Orthodontics
Orthodontics is one of the most dynamically developing field of dentistry, and the first separate specialty that was formed within dentistry. Orthodontics deals with the diagnosis, the progression and the treatment of morphological and positional irregularities of the teeth, the alveolar ridge and the jaw bones. Orthodontics is more than achieving proper tooth alignment: an aesthetic smile with proper function also requires correct relationship between the two dental arches and a healthy jaw joint to provide a firm frame for this. Orthodontists need complex knowledge to take appropriate diagnostic measures, to evaluate the individual characteristics of the patients, and to inform them about the treatment plan that meets their needs. An interdisciplinary approach is required, which can utilise the benefits of maxillofacial orthopaedics in order to provide a durable and successful outcome without making compromises. Responsible orthodontics is aimed at the early diagnosis of abnormalities, their regular follow-up, and if needed, preventive treatment to correct the development of the jaw bones. After the desired outcome has been achieved, it must be preserved and maintained. Patients with complete dental development may require skeletal anchorage or maxillofacial-orthopaedic surgery to correct orthodontic abnormalities that affect their fully developed jaw bone and dental arch.
Why is it important to undergo orthodontic treatment?
Orthodontic treatment is not only about aesthetics, it has an important role to restore your chewing function. Irregular bite can lead to difficulty chewing, speaking, or breathing. Improper contact between the teeth can lead to overload and, eventually, tooth loss. Abnormal occlusion (bite) can cause problems affecting the jaw joint (e.g. pain or clicking). Crowding of the teeth can make it difficult to clean, which can result in gingivitis or tooth decay. Therefore, the purpose of orthodontic treatment is to eliminate these problems by creating proper alignment of the dental arch.
The most common types of abnormalities affecting the teeth, the bite and the jaw bone.
Causes:
Irregular bite is most frequently caused by genetic factors. Parents with irregular teeth are likely to pass it on to their children. However, parents with healthy teeth may also have children with orthodontic abnormalities. These types of abnormalities are called congenital defects, and they include cleft lip or palate, supernumerary teeth, absence of dental germs, distorted teeth, or abnormal upper or lower jaw development. Orthodontic problems can also be brought on by mechanic effects caused by lifestyle factors or certain habits, such as prolonged pacifier use or bottle feeding, finger sucking, or tongue thrusting (abnormal position and function of the tongue when swallowing). Dental trauma and improper oral hygiene in childhood can result in early loss of the temporary teeth, which can influence the normal process of tooth shedding.
Absence of dental germs
This condition is usually genetic, but external factors, including infections, medications or trauma, can also contribute to it. It can affect milk teeth, especially front teeth, but permanent teeth can also be affected leading to the absence of upper lateral incisors, lower first premolars, second molars or wisdom teeth.
Supernumerary teeth:
Extra teeth can develop if the tooth germ splits (these teeth are likely to grow smaller and misshaped), or you develop more tooth germs than normal. Supernumerary teeth are usually found among the permanent teeth in the upper jaw at the front, however, some patients can have extra milk teeth. Supernumerary teeth can be of normal size and shape, but they can also be smaller and misshaped. The most common type of supernumerary teeth is called mesiodens. It develops between the upper front teeth, leaving a gap between the upper central incisors, or even blocking their normal eruption. Supernumerary teeth can damage the roots of the neighbouring teeth and make them displaced, which can eventually lead to aesthetic problems or difficulties with speech.
Diasthema (gaps between the teeth):
Diastema is most common between the upper front teeth, and it is not only an aesthetic problem, but it can also affect the formation of speech sounds. Gaps are usually caused by abnormal dental development, missing tooth germs, unerupted supernumerary teeth, or excessive stretching of the upper labial frenulum.
Crowding:
Crowding occurs if the permanent teeth cannot erupt into their normal position in the dental arch. Crowding is most prominent in the area of the front teeth. The condition can make tooth brushing difficult, thus the risk of developing gingivitis or tooth decay is increased.
Transposition:
Transposition occurs when two teeth, for example the upper first premolar and the canine, change places in the dental arch. The condition is usually due to abnormal tooth shedding.
Impaction:
An impacted tooth is a tooth which is blocked in the jaw and cannot erupt. The blockage that prevents eruption can be a supernumerary tooth, or another tooth which is in normal position, but has become tilted because of the abnormal position of its dental germ. This condition usually affects wisdom teeth or upper canine teeth.
Retention:
Retention occurs when the dental germ cannot break through, in spite of the fact that there is no obvious blockage.
Ectopic teeth:
An ectopic tooth is a tooth which is located outside the dental arch. Most of the time upper canines and lower second premolars are affected.
Cross bite
Cross bite usually occurs in the incisor area, when the lower incisors bite in front of the upper ones. Cross bite can affect more than one tooth, both in the frontal region and in the lateral zone.
Open bite
Open bite occurs when there is no contact between certain upper and lower teeth, or groups of teeth, when you close your teeth. One of the most common causes of open bite is bad habits (pacifier use, finger sucking).
Overbite
Overbite is present when the edge of the upper incisors deeply overlaps the lower incisors. In patients with severe overbite, the upper edge of the lower incisors bites into the gum behind the upper incisors. This bite disorder can often lead to periodontal problems later on.
Protrusion
Protrusion (buck teeth) is an orthodontic condition, where the front teeth are leaning outwards.
Retrusion:
Retrusion is an orthodontic condition, where the front teeth are leaning inwards.
Edge-to-edge bite
Edge-to-edge bite is found when the upper and lower incisors do not overlap, but meet at the biting edges.
Asymmetry
Asymmetry can occur within the dental arch, at the level of the dentition, involving the jawbones and the soft tissue. Asymmetry occurs when the middle planes of the upper and lower incisors are not in the same line, i.e. the midline is shifted. If this irregularity is not corrected in time, it can lead to severe deformities, even affecting the whole face.
Micrognathia
Micrognathia is present when the upper jaw (maxilla) is undersized or falls behind the lower jaw.
Microgenia
Microgenia is present when the lower jaw (mandible) is undersized or falls behind the upper jaw.
Prognathia
In prognathia the upper jaw (maxilla) is oversized or falls in front of the lower jaw.
Progenia
In progenia the lower jaw (mandible) is oversized or falls in front of the upper jaw.
Orthodontic treatment in childhood
 Regular dental check-ups for children are important, as early detection of any changes that may require orthodontic treatment is important. Keeping the mouth slightly open, obstructed nasal breathing and speech problems can be warning signs. It is therefore recommended to take children for an initial consultation at the age of 6-7 years. At this time the dentist will assess the growth trend and the expected time for the teeth to erupt, and screen for any abnormalities due to bad habits in childhood. It is not necessary to wait for all the milk teeth to fall out, treatment with a removable appliance can be started before that. This is the most effective period to influence and control the growth of the jaws. The treatments which affect both jaws are known as functional or maxillofacial-orthodontic treatments. If these treatments are not performed in time, some abnormalities can only be corrected later by surgical methods. The removable appliances can be used to adjust the bite and correct irregular jawbone conditions. Depending on the specific problem, several types of appliances can be used. Removable appliances are often called night-time appliances, but it is not entirely correct, because it is not enough to wear them only at night. These appliances must be kept in the mouth for at least 12-14 hours to take effect. The second stage of treatment involves fitting a fixed appliance to adjust the occlusion, although certain conditions can be corrected with removable appliances alone.
Regular dental check-ups for children are important, as early detection of any changes that may require orthodontic treatment is important. Keeping the mouth slightly open, obstructed nasal breathing and speech problems can be warning signs. It is therefore recommended to take children for an initial consultation at the age of 6-7 years. At this time the dentist will assess the growth trend and the expected time for the teeth to erupt, and screen for any abnormalities due to bad habits in childhood. It is not necessary to wait for all the milk teeth to fall out, treatment with a removable appliance can be started before that. This is the most effective period to influence and control the growth of the jaws. The treatments which affect both jaws are known as functional or maxillofacial-orthodontic treatments. If these treatments are not performed in time, some abnormalities can only be corrected later by surgical methods. The removable appliances can be used to adjust the bite and correct irregular jawbone conditions. Depending on the specific problem, several types of appliances can be used. Removable appliances are often called night-time appliances, but it is not entirely correct, because it is not enough to wear them only at night. These appliances must be kept in the mouth for at least 12-14 hours to take effect. The second stage of treatment involves fitting a fixed appliance to adjust the occlusion, although certain conditions can be corrected with removable appliances alone.
Orthodontic treatment for adults
Orthodontic treatment is also available for adults. First impressions are important in human relationships, and a harmonious, confident smile reflects positive energy. In addition to aesthetic needs, medical and health considerations are also very important. Adult orthodontic treatment may be necessary to prepare for replacements, when there is not enough space for an implant and the aim is to open a gap with braces, to straighten teeth tilted into a gap left by a missing tooth, or to eliminate frontal crowding, and there are many other cases where orthodontics may be the solution. Today, a wide range of appliances and technologies are available, depending on the severity of the abnormality and the treatment goals. The harmonious relationship between a perfectly aligned dentition and the jaw bone is a prerequisite for normal oral function and prolonged oral health, without tooth decay and periodontal disease. Orthodontic treatment in adults can correct abnormal function at an older age with excellent results. However, it is important to know that since jaw bone growth is no longer expected at this stage, correct treatment of a complex dento-skeletal abnormality affecting the jaw bone may sometimes require surgical reposition of the jaw.
What is needed for the success of an orthodontic treatment?
In addition to a precise treatment strategy defined by the excellent and constantly expanding expertise of the orthodontist, patient cooperation, regular visits to the dentist and perfect oral hygiene are essential for the success of the orthodontic treatment. It is important that patients take care of their appliance, and do not hinder or slow down the changes that are taking place. Orthodontic treatment requires patience on both sides and cannot be rushed, as bone breakdown and remodelling that occurs when the teeth are moved is biologically determined. Proper communication, understanding and motivation are essential to encourage the patient during this long-term collaboration.
Orthodontic appliances
There are various types of orthodontic appliances, depending on the abnormality to treat. There are two broad groups of appliances: fixed and removable, with several types within each.
Removable appliances are orthodontic appliances that can be easily removed by the patient. They have the advantage of being easy to clean and not interfering with oral hygiene, they are less visible and, most importantly, they can be used to positively influence the development of the jaw bone in childhood. However, they require a great deal of patient cooperation, as adequate wearing time (12-14 hours a day) is essential for them to be effective. These appliances are usually made of plastic, but may also contain other metal parts (labial arch, wire clips, screws, etc.). There are so-called passive plates, which are used to maintain a given state, and appliances with active elements. Functional, also known as bimaxillary, devices are attached to both dental arches. They transmit the force of the chewing muscles to the teeth and the periodontium, and influence the growth of the jawbones.
The best known and most sophisticated group of fixed appliances are the multibracket systems. The multibracket systems require the presence of permanent teeth. Partial appliances can be attached if the first molars and four incisors have erupted.
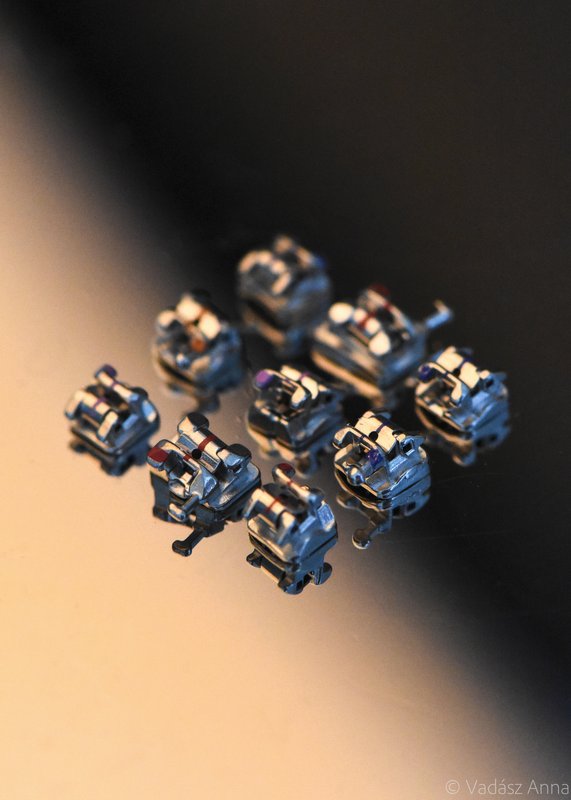
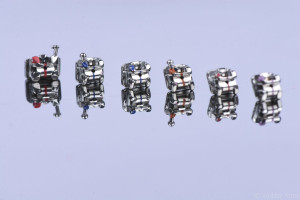
They can be classified according to the ligation method: traditional/self-ligating (active and passive), the bracket material: metal/aesthetic (plastic, ceramic, sapphire crystal), and the location: labial (on the outer surface of the teeth)/lingual (on the inner surface of the teeth).
Parts of the multibracket systems
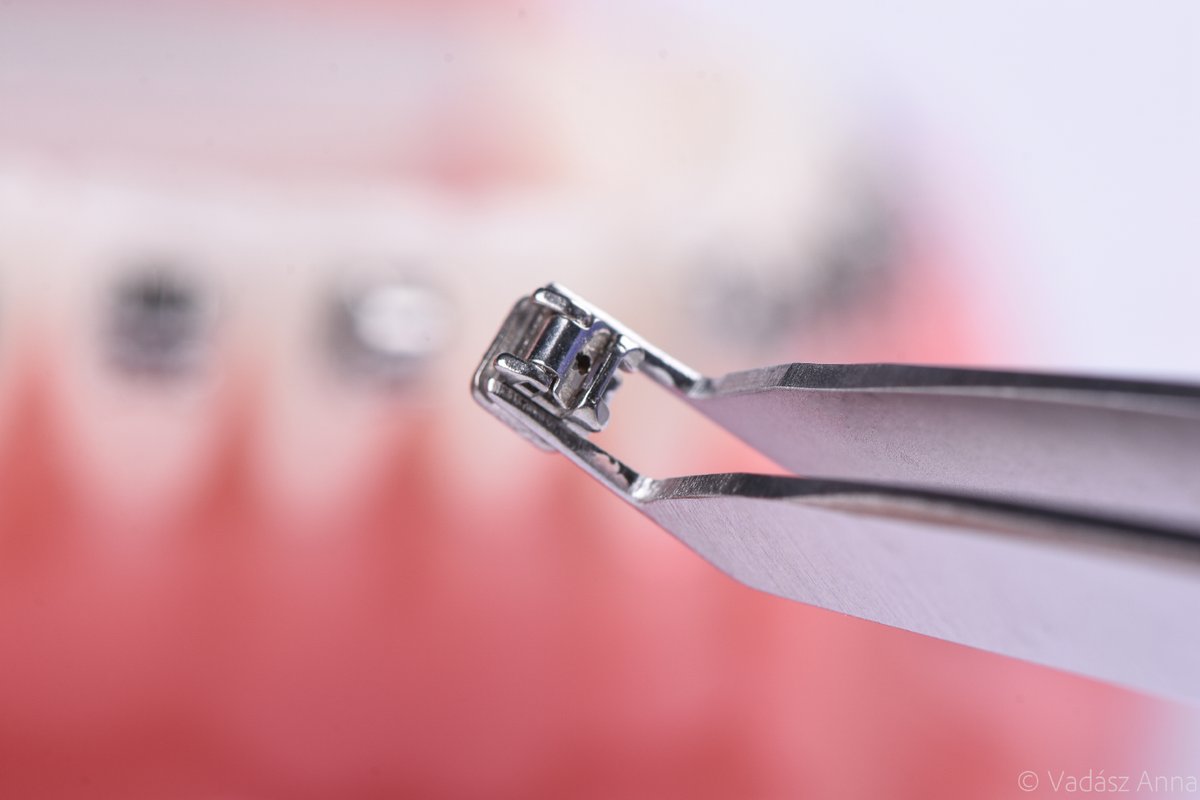
Bracket – The brackets are those parts which are bonded to the outer or inner surface of the teeth. They are responsible for transmitting the forces exerted by the arches that move the teeth. Brackets contain a special slot to accommodate the arches, the design of which is unique for each tooth depending on the direction of movement. The arch is secured in the slot by an elastic/steel ligature (conventional systems) or a clip (self-ligating systems), which can be active or passive.
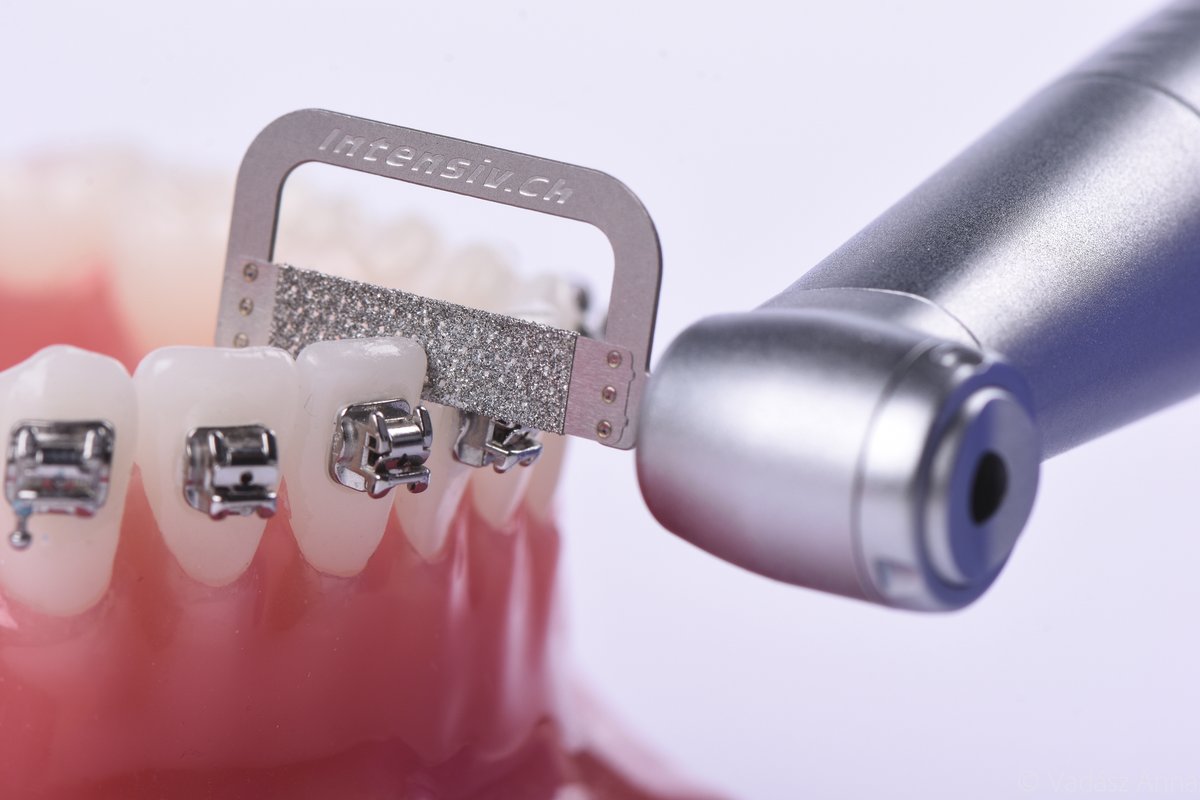
Arch – In the first phase of the treatment, the arch is made of a circular elastic material. In later phases, the diameter of the arch increases, the cross-section changes from circular to square and then rectangular. When the arch is replaced, the old arch is removed and the next type of arch is secured. In the case of conventional systems, the procedure also involves the replacement of old ligature devices with new ones. With self-ligating systems, replacing the arches takes much less time. The clips are opened, the new arch is inserted into the slot, and the clips are closed again to secure the arch. Rigid arches, used in certain treatment phases, can accommodate individual bends, which allow for the movement of individual teeth in specific directions and to specific degrees. The arch should be correctly attached, it should extend into the slot of the tooth to be moved, it should not poke the inside of the cheek, and that it should not be too long. Slipping of the arch can be prevented with stops.
The steps of the orthodontic treatment
1. First consultation:
The first consultation takes place by appointment, and the patient’s needs and the goal to be achieved are discussed. A detailed dental examination will be performed, including a functional examination. The patient’s oral hygiene and the condition of the teeth are also assessed. In order to start an orthodontic treatment, it is essential to have perfect oral hygiene and to treat existing cavities, unhealthy teeth and teeth with complaints, as cleaning and further dental treatments (e.g. filling) become more difficult after the appliance has been fitted.

2. Second appointment, documentation:
Documentation will take place at the second appointment: X-rays, photographs and impressions are taken and evaluated to determine a precise treatment plan. It is important that the patient has a good oral hygiene and healthy dentition, because without this, the documentation cannot take place.

3. Discussing the treatment plan:
This is the time for a detailed discussion of the treatment plan and the prices. Everything must be clear to the patient, so great emphasis is placed on communication. If the patient agrees to the treatment, the process of ordering the appliance starts.
4. Handing over and fitting the orthodontic appliance:
This is when the orthodontic appliance is handed over and fitted. The fixed appliance may take longer to be fitted. The brackets are bonded to the tooth surface with an adhesive material that sets immediately in response to the light of a special lamp. This is done in such a way and with such force that the teeth are not damaged when the appliance is removed at the end of the treatment. It is therefore very important that patients take care of their orthodontic appliances. The dentist will teach the patients how to clean their teeth and the appliance, and demonstrates the methods on a model. It is forbidden to bend or force any parts the appliance by hand or with an instrument, and to eat hard/sticky foods (biting, chewing). Any damage to the appliance should be reported to the dentist so that further actions can be taken. It is recommended to brush the teeth and rinse the mouth after main meals. Patients should buy and use an interdental brush to clean the areas between brackets and under the arch. Dentists should warn their patients, that for some time, until they get used to wearing the appliance, tooth sensitivity and pain can occur. Protruding parts of the appliance can cause irritation of the oral mucosa and, in more serious cases, even injury. In such cases, the application of wax is recommended and the patient should be instructed in its use at the time of bonding. Likewise, practical training is required to learn how to apply the rubber band between the two jaws at a later stage of the treatment, and to practise the use of a special aid in front of a mirror. For patients with fixed orthodontic appliances regular (monthly) check-ups should be scheduled.
5. Activation, setting the braces:
Depending on the appliance, the braces should be activated and adjusted at a regular interval (usually monthly for multibracket systems). At these visits an orthodontic check-up is performed, and, if necessary, the arch is replaced, and elastic parts and springs are fitted. After activation, tooth sensitivity can be expected for a few days.
6: Finishing the orthodontic treatment
When the treatment has achieved its purpose and the correct tooth contact has been established, the orthodontist removes the appliance. A fixed retention appliance, which is made on the basis of the impressions taken beforehand, is fitted at the time of removal, usually from canine to canine, on the inner surface of the lower and upper teeth. The retainer is used to maintain the condition achieved. The fixed retainer needs the same care, it requires proper cleaning, but within a few days the patient gets used to its presence. Once the retainer has been fixed, another impression is taken for the dental technician to fabricate a removable retainer. The removable appliance should be worn overnight, usually for 1-1.5 years after the active phase is completed. At the end of the treatment, photographs are taken and finishing models are made again.
7. The passive, retention phase and its monitoring:
It is important to check both the removable and the fixed retainers regularly, because if there are any problems with them, the orthodontist can correct them and replace them if necessary. It is important to monitor the results achieved, which can be analysed by taking additional images and comparing them.
Risks of orthodontic treatment
Like all medical procedures, orthodontic treatments can have risks. However, by recognising and considering them, most of the risks can be consciously avoided or prevented.
Changes in caries activity, decalcification, discolouration, pulp damage: One of the risks is the appearance of white spots (the initial stage of caries, white spot lesions), which can be reversed. It occurs mainly on the outer surface of the front and lateral teeth of the upper dental arch. Factors that increase the risk of developing this condition include existing decalcification stains, inadequate oral hygiene, inadequate education and dental care advice, or poor diet. Preventive measures can be the use of fluoride ion-releasing bracket adhesives, topical fluoride products (varnishes, mouth rinses), CPP-ACP complex, thorough tooth cleaning, and good oral hygiene.
Gingivitis: Gingivitis is a common complication of fixed orthodontic appliances. It can be caused by plaque (sticky deposit), as well as by local irritants (brackets). Fixed orthodontic appliances can increase the surface to be cleaned leading to difficulty in maintaining good oral hygiene. Gingivitis usually starts at the tip of the gingival papilla as a bright red, then dark livid area. The orange-peel appearance of the attached gums is smoothed by oedema, and an increased tendency to bleed, excessive production of gingival secretions and pseudo-pocket formation are present. By eliminating the causes, the process can be reversed. If the condition persists for a long time, it can lead to fibrotic thickening of the gums. Preventive measures include oral hygiene education, regular check-ups, and regular professional cleaning.
Gingival recession: Tooth movement does not directly cause gingival recession, but it can create an environment that increases the risk in susceptible individuals: if the tooth is not covered by cortical bone. Recession develops in areas where the alveolar ridge is the thinnest and the root surface is the most prominent (outer surface of the lower incisors and canines, inner surface of the upper molars) Factors that increase the risk of developing gum recession include thin gingival biotype, dehiscentia, forceful brushing, overloading the teeth (e.g. bruxism), or inflammation caused by plaque. Gingival recession is more commonly observed during adult orthodontic treatment (reduced regenerative capacity). In order to avoid gum recession, the thickness of the cortical bone plate must be examined (X-ray, CBCT) and the degree of tooth movement must be planned precisely before the treatment.
Loss of attachment
Bone and root resorption: Orthodontic treatment is based on the remodelling of the bone and the root due to the force exerted on the teeth. Severe root resorption can occur when body’s regenerative processes are unable to make up for the loss of cementum and dentin, or when the degree of resorption due to pressure is so extensive that the root tip is essentially separated from the rest of the root. Typically, resorption affects the root tip, but it may also involve the areas around the tip. Factors that increase the risk of resorption can be conical, pointed roots, previous trauma, root canal treatment, short anatomical root length, or previous orthodontic treatment. Resorption can be prevented by regular radiological control, and the use of smaller forces and even distribution.
Mucosal injuries, allergological aspects, Candida infection
Jaw joint dysfunctions