Root canal treatment can save teeth
About root canal treatment
Root canal treatment is a dental intervention performed to save a tooth if the pulp, which is the innermost layer of the tooth, is irreversibly damaged. There are several dental conditions that require root canal treatment, such as extensive decay, trauma, gum disease, abrasion (loss of enamel due to mechanical forces), or erosion (loss of tooth structure due to acids), and your dentist will reveal the exact cause. The intervention must be performed by an expert team, because later on teeth with root canal treatment can serve as anchors for tooth replacements, which is often the case in a dental surgery offering complex dental treatments. Root canal treatment at Dentoplant Dental and Implantological Clinic is performed using modern pain control methods and high professional standards.
Toothache and inflammation of the pulp
When the pulp of your tooth is inflamed, eating or drinking something hot or cold can make you feel a sudden, sharp pain that lasts for minutes. If the inflammation is widespread, the pain can occur without any external impact. For example, many patients report pain that wakes them up at night and it cannot be relieved with painkillers. On the other hand, if the pulp is dead due to permanent inflammation, you may not have any symptoms. When your tooth is dead, it cannot defend itself and the bacteria in the tooth increase and cause chronic inflammation that can spread to the tip of the root and the deeper tissues. Acute inflammation of the root tip (apex) can cause sensitivity or pain when you chew or bite, or it can even lead to an abscess, collection of pus around the tip. If left untreated, the abscess can cause severe complications. Chronic inflammation around the root tip usually remains unnoticed and is only revealed on routine X-rays. Dead teeth can result in a so called focal infection.
Oral focal infection
Oral focal infection is a chronic inflammation around the teeth which may not produce any symptoms in the mouth. These inflamed areas can release pathogens (germs) or toxins (poisonous substances) that can get into other organs. Teeth are not the only sources of such infections, which can spread from the tonsils, the sinuses, the ovaries, the gall bladder, the appendix or the prostate. Depending on the pathogen or the toxin and the target organ, the infection can cause other medical conditions, such as patchy hair falling, eczema, allergic skin rashes, eye infection, arthritis, vessel inflammation or kidney infection.
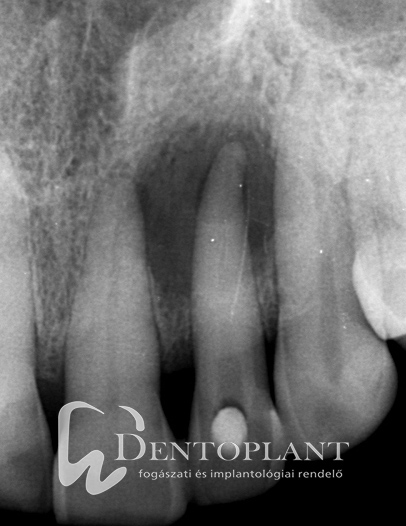
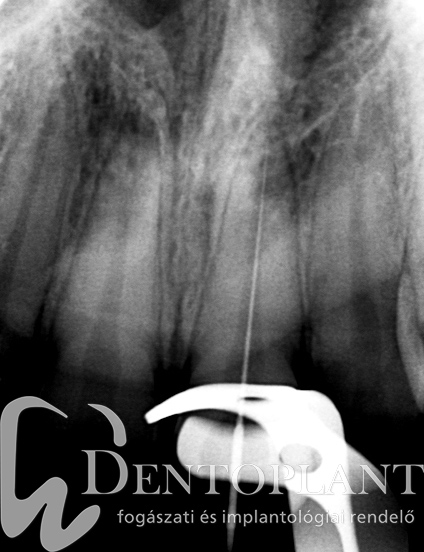
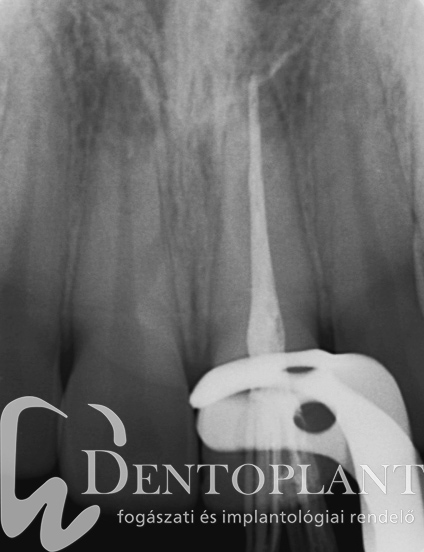
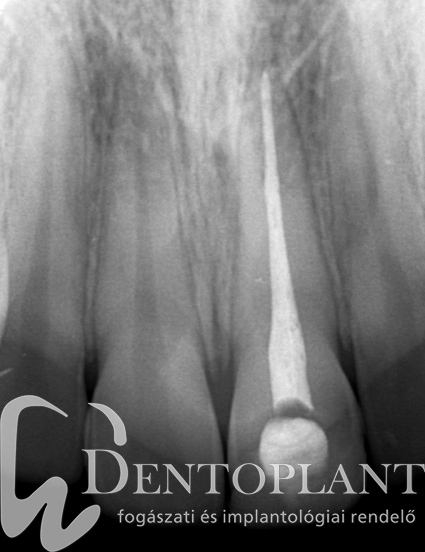
Picture 1, 2, 3 Collection of pus around the tip of the upper left small incisor did not cause any symptoms, it resolved within ten months after root canal treatment.
The steps of root canal treatment
Root canal treatment involves removal of the pulp, cleaning of the cavity using mechanical and chemical methods, and filling the cavity. The treatment usually requires more than one visits to the dentist.
Your dentist removes the pulp and the infected dentine (hard tooth material) and shapes the cavity so that it can be filled. The first step is numbing your tooth. Then your dentist opens your crown to make the pulp chamber and the entrance to the root canal visible and accessible. The shape and structure of the roots and the root canals vary widely, therefore it may be difficult to find and clean them properly.
Rubber dam isolation
A rubber dam is a thin sheet of rubber used to isolate the treated tooth or teeth from the oral environment, to prevent the migration of bacteria from your saliva into the root canal, and to provide a dry, clean and visible area for root canal treatment. Occasionally it might be necessary to build up the tooth and create a so called temporary endodontic restoration stump prior to root canal treatment.
Mapping the root canals
Proper root canal treatment and filling must include all root canals and the entire length of the canals down to the narrow tip of the root. Although X-ray images of your tooth can be useful, exact visualisation of the whole system of root canals is only possible using a 3D CT scan. Modern CT scans can be targeted to the affected tooth, so your dentist can minimise your exposure to radiation.
Picture 4 Modern diagnostic methods, such as CBCT scans in root canal treatment.
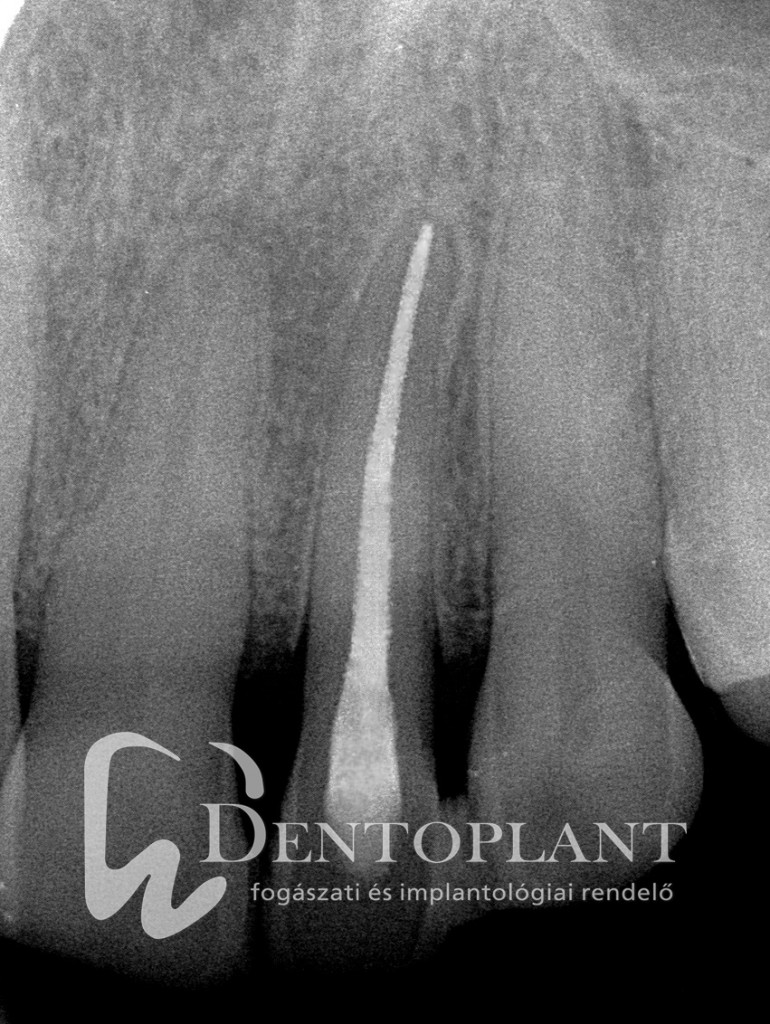
Establishing the working length
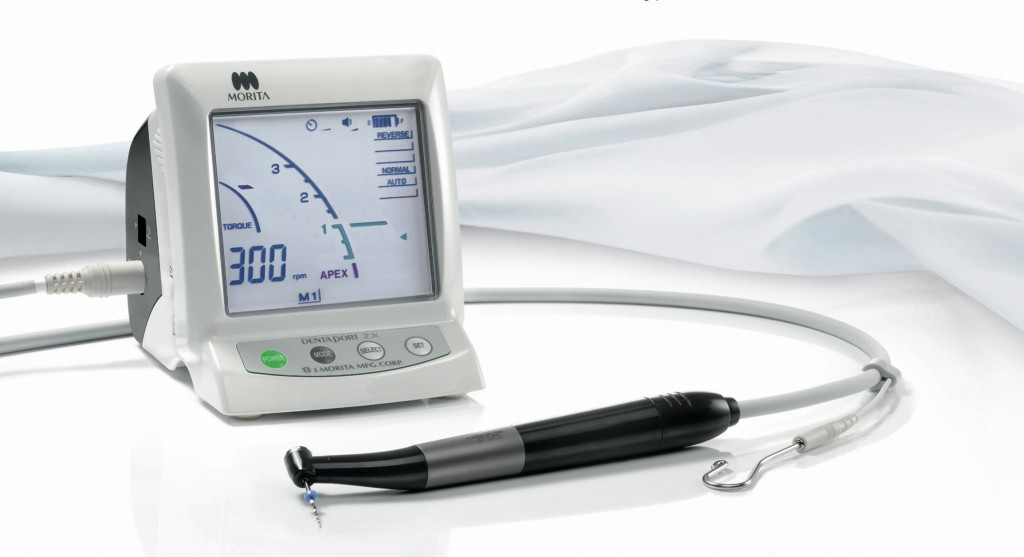
The working length is usually established using an X-ray image of the tooth and an apex locator, which is an endodontic device that can measure the length of the root canal. The X-ray image is taken with an endodontic file placed into the root canal. This image can help your dentist to estimate and clean the whole length of the root canal. The apex locator measures the electric impedance between the soft tissues of your mouth and the apical periodontium, the area around the tip of the root, which is a constant value. Our clinic uses MoritaDentaPortZX© system to measure and shape the root canal.
Modern root canal treatment with MoritaDentaPortZX© handpiece
There are several types of hand files and electric files based on their conicity (tapering shape) and the preparation technique (shaping of the root canal) they are used for. Besides conventional hand files we use state-of-the-art MoritaDentaPortZX© handpiece with Endowave© and ProTaper Next© files to shape and clean the root canal quickly and properly. Each patient requires an individual approach, therefore, in order to provide the best treatment for you, your dentist will decide which instrument and which preparation technique to use based on your individual condition. No matter how modern and effective files your dentist will use, mechanical preparation should be combined with irrigation of the root canal. Studies have found that certain areas in complex root canal systems and narrow side canals cannot be reached with shaping the canals, they can only be accessed with irrigation.
After shaping and cleaning the root canal, your dentist will place an antiseptic dressing containing calcium-hydroxide into the root canal and close the tooth with a temporary filling. The treatment is usually completed at the next visit.
Picture 5, 6 DentaPort ZX© handpiece
The steps of root filling
The purpose of filling the root is to seal the pulp chamber and prevent the accumulation of bacteria. The shaped and cleaned canals are filled with a rubber-like material called gutta percha and a fine sealing paste that can be compacted into the tiny crevices. There are various filling techniques and materials. There are techniques that use cold filling material, such as pre-fabricated gutta percha cones, and apply lateral (sideways) or vertical compression to fill the canal. Other techniques use heated, thermoplastic materials. These materials are either injected into the canal or delivered with a special cylinder. The root canal can also be filled using the so called heating – compression method, when gutta percha pellets are inserted, heated and compressed step by step until the whole canal system is filled.
The most common filling technique is lateral compression with cold gutta percha cones. First, an X-ray is taken with gutta percha cones used as reference. Your dentist chooses a gutta percha cone for each prepared canal. The length of the cone is the same as the length of the file last used to shape the canal. The X-ray image with the cone inside the root canal can help your dentist decide about the proper length of the filling. Then the dentist dries the canal, inserts a sealer and a cone and compresses the filling material sideways using a hand spreader. After that further cones are inserted and compressed into the canal until the whole length is filled. Another X-ray is taken to check if the canal is filled properly, then your dentist removes excess filling material from inside the crown. Finally, the crown is closed with a temporary filling, because it takes 2-3 days for the root filling to set.
Picture 6, 7, 8 Phases of root canal treatment using rubber dam isolation: initial X-ray with file reference, preparation of permanent filling, complete filling
Restoration of teeth after root canal treatment
The key to successful root canal treatment is preparing a durable restoration that seals the crown and prevents the tooth from bacterial re-infection. It is also essential to strengthen the remaining tooth material, because after root canal treatment there is no circulation in the tooth, it becomes dry and brittle, and can eventually break.
There are various methods to restore the tooth depending on the extent of the damage, the location of the tooth in the dental arch, and the condition of the tooth on the opposite side. Modern restoration methods rely on biomimetics, which means that lost tooth materials are replaced with artificial materials that possess similar properties. For example, dentine (the hardest part of the tooth) and enamel are replaced with different materials. If the tooth is badly damaged and has lost a lot of dentine, it is strengthened with a glass-fibre post. After careful preparation the post is fixed both into the root and the crown, and it can distribute the forces exerted on the tooth and make the tooth stable. Tooth enamel can be replaced with tooth-coloured materials or golden inlays, onlays or overlays. Depending on the damage the crown can be restored with a composite (aesthetic) filling or an artificial crown made of metal-ceramics or aesthetic metal-free zirconium.
Picture 9, 10 Following root canal treatment with rubber dam isolation we insert a glass-fibre post and make a permanent restoration
Endodontic retreatment: the last resort to save a tooth
Endodontic retreatment is repeating faulty root canal treatment. This is the last chance to treat a tooth before your dentist performs a surgical intervention to save or remove it. Retreatment usually involves replacing a faulty, ill-fitting or incomplete filling. What is an incomplete filling? The filling is considered incomplete if it is too short and does not reach the tip of the root, or it does not fill or seal the cavity.
The first step of retreatment is removing the old filling and correcting any deficiencies that have lead to the failure of the previous root canal treatment. Such deficiencies can include a root canal that has not been revealed, incomplete shaping and irrigation of the root canal, or miscalculated working length. Then the root canal is disinfected several times by inserting a medicinal paste with calcium-hydroxide into the canal. Retreatment is essential if the tooth is still painful two months after the treatment (sensitivity on biting is only acceptable within two month of treatment), if swelling, fistulas (gumboil) or periapical lesions (collection of pus around the root) occur, if the crown restoration does not seal properly, or if it is not placed after root canal treatment and the tooth gets re-infected by bacteria. If the reason for the first root canal treatment was a periapical abnormality (chronic periapical periodontitis), close follow-up is required to observe the abnormality. Root canal treatment fails if the abnormality does not resolve, or even progresses, within 4 years.
Your dentist may recommend retreatment even if you do not have any complaints and a routine X-ray reveals a faulty filling, or the tooth will be used as an anchor for restoration, or an implant will be placed next to the tooth. These circumstances in the presence of periapical abnormality make root canal treatment indispensable. A faulty root filling can cause further inflammation, which can lead to the failure of subsequent restorations or implants. The final step of retreatment is inserting a permanent filling and restoring the crown.